2021-2022 Choices Retiree Workbook
Retiree Benefits 2021-2022
Montana University System

 Table of Contents
Table of Contents
- Campus Human Resources/Benefit Office Contacts
- Enrolling as a Retiree
- Retiree Rates
- Medical Plan Costs
- Schedule of Medical Benefits
- Preventive Services
- Prescription Drug Plan
- Dental Plan
- Vision Hardware Plan
- MUS Wellness Program
- Additional Benefit Plan Information
- Glossary
- Insurance Card Examples
- Resources
Campus Human Resources/Benefits Office Contacts
920 Technology Blvd, Ste. A,
Bozeman, MT 59717
406-994-3651
MSU - Billings
1500 University Dr.,
Billings, MT 59101
406-657-2278
MSU - Northern
300 West 11th Street,
Havre, MT 59501
406-265-3568
Great Falls College - MSU
2100 16th Ave. S.,
Great Falls, MT 59405
406-268-3701
UM - Missoula
32 Campus Drive, LO 252,
Missoula, MT 59812
406-243-6766
Helena College - UM
1115 N. Roberts,
Helena MT 59601
406-447-6925
UM - Western
710 S. Atlantic St.,
Dillon, MT 59725
406-683-7010
MT Tech - UM
1300 W. Park St.,
Butte, MT 59701
406-496-4380
OCHE, MUS Benefits Office
560 N. Park Ave,
Helena, MT 59620
877-501-1722
Dawson Community College
300 College Dr.,
Glendive, MT 59330
406-377-9430
Flathead Valley Community College
777 Grandview Dr.,
Kalispell, MT 59901
406-756-3981
Miles Community College
2715 Dickinson St.,
Miles City, MT 59301
406-874-6292
Choices Enrollment for a Retiree
To select Choices benefit options as a Retiree, you must complete and return a Retiree Enrollment Form to your campus Human Resources/Benefits Office to make your benefit elections:
- within 63 days of retirement and becoming eligible for Retiree benefits. If you do not enroll within the 63-day enrollment period, you will permanently forfeit
your eligibility for all Retiree insurance coverage.
- during annual enrollment by the stated deadline. If you do not make any benefit changes, you will be automatically enrolled in your
current benefit elections and coverage levels or to the stated default coverage if
your existing plan(s) is/are changing.
- when you have a mid-year qualifying event (marriage, birth or adoption of a child, loss or gain of eligibility for other health insurance coverage - voluntarily canceling other health insurance does not constitute loss of eligibility) and want to make an allowed mid-year change in benefit elections. This change must be made within 63 days of the event. Documentation to support the change will be required.
MEDICARE ENROLLMENT: Retirees and/or their covered dependents who are or become Medicare-eligible (age
65) at retirement or after, must be enrolled in BOTH Medicare Part A and Medicare Part B. If Medicare enrollment is not completed within
sixty-three (63) days from the date of the employee’s retirement or retiree’s or covered
dependent’s Medicare eligibility date, the individual(s) will be disenrolled from
the MUS Choices Medical and Prescription Drug Plans. Enrollment in the Select Dental
Plan and/or Vision Hardware Plan may be continued if the Medicare-Eligible Retiree
is enrolled in those plans at retirement or on the date of Medicare eligibility even
if they are disenrolled from the MUS Choices Medical and Prescription Drug Plans due
to not enrolling in Medicare Part A and Part B.
No Retreat Rights:
If you decline Retiree Medical, Dental, and/or Vision Hardware plan coverage(s), you and your eligible dependents will permanently forfeit your coverage(s) and will NOT be allowed to enroll in the future.
If you are declining coverage for your eligible dependents (including your legal spouse), as those persons are defined by the Montana University System (MUS) Summary Plan Description (SPD) because they are currently covered by another health insurance plan, you may be able to enroll your eligible dependents for coverage under the MUS Plan in the future, provided you request such coverage within 63 days after their other coverage ends.
If you acquire an eligible dependent, as defined by the MUS Plan, due to marriage, birth, adoption, or placement for adoption of a child under the age of 18, you may enroll your newly acquired dependent child(ren) or legal spouse for coverage under the MUS Plan, provided that such enrollment occurs within 63 days after the marriage, birth, adoption or placement for adoption.
Reminder: Enrollment for FY2022 is Closed Enrollment for legal spouses unless there is a qualifying event (see Summary Plan Description (SPD) for qualifying events).
Step-by-Step Process for Completing Your Choices Retiree Enrollment Form
Step 1: Review this workbook carefully and read the back of the Retiree Enrollment Form
- Discuss this information with your legal spouse and/or other family members.
- Determine your benefit needs for the coming benefit plan year if you are enrolling during annual enrollment or for the remainder of the current benefit plan year if a new Retiree.
Step 2: Complete your Retiree Enrollment Form.
Your Retiree Enrollment Form should be included with this workbook. In the event your enrollment form is missing, or you need another copy, please contact your campus Human Resources/Benefits Office (pg 3).
Medical Coverage
For Medical coverage, you must be qualified to enroll (see back of enrollment form). If you do not make an election to continue your Medical coverage when you first retire, you will permanently forfeit your Medical coverage.
- Choose the coverage level you want.
- Once you have selected a coverage level, fill in the corresponding monthly premium in the space provided on the right-hand side of the enrollment form, by “Medical Premium”.
- or check the box that declines Medical coverage entirely.
Medicare Retiree Prescription Drug Coverage
- Medicare Retirees will be automatically enrolled in the Navitus MedicareRx Plan.
- If you opt out of the Navitus MedicareRx Plan or get another Medicare Part D plan, you will forfeit your MUS Medical Plan benefits.
Dental Coverage
For Dental coverage, you must be qualified to enroll (see back of enrollment form). Retirees are offered enrollment in the Select Dental Plan only. If you do not make an election to continue your Dental coverage when you first retire, you will permanently forfeit your Dental coverage.
- Choose the coverage level you want.
- Once you have selected a coverage level, fill in the corresponding monthly premium in the space provided on the right-hand side of the enrollment form, by “Dental Premium”,
- or check the box that declines Dental coverage entirely.
Vision Hardware Coverage
For Vision Hardware coverage, you must be qualified to enroll (see back of enrollment form). If you do not make an election to continue your Vision Hardware coverage when you first retire, you will permanently forfeit your Vision Hardware coverage.
- Choose the coverage level you want.
- Once you have selected a coverage level, fill in the corresponding monthly premium in the space provided on the right-hand side of the form, by “Vision Premium”,
- or check the box that declines Vision Hardware coverage entirely.
Step 3: Demographic and Dependent Coverage.
Please fill in these sections completely every time you fill out the Retiree Enrollment Form.
Total Your Costs: Add up the premium amounts and enter the total on the Total Monthly Premium line.
If you have not arranged with your campus Human Resources/Benefits Office for automatic payment of your premiums through your pension plan, it is strongly recommended that you consider doing so.
How the Choices Medical Plan Works
Plan members receive medical services from a health care provider. If the provider is In-Network, the provider will submit a claim for the member. The Medical Plan claim’s administrator processes the claim and sends an Explanation of Benefits (EOB) to the member and the provider, showing the member’s payment responsibilities (deductible, copayments, and/or coinsurance costs). The Plan then pays the remaining allowed amount. The provider will not bill the member the difference between the billed charge and the allowed amount.
If the provider is Out-of-Network, the member must verify if the provider will submit the claim or if the member must submit the claim. The Medical Plan claim’s administrator processes the claim and sends an EOB to the member showing the member’s payment responsibilities (deductible, coinsurance, and any difference between the billed charge and the allowed amount (balance billing).
Definition of Terms
In-Network Providers – Providers who have contracted with the Plan claim’s administrator to manage and deliver care at agreed upon prices. Members may self-refer to In-Network providers and specialists. There is a cost savings for services received In-Network. You pay a $30 copayment for Primary Care Physician (PCP) visits and a $50 copayment for Specialty provider visits to In-Network providers (no deductible) and 30% coinsurance (after deductible) for most In-Network hospital/ facility services.
Out-of-Network Providers – Providers who do not have a contract with the Plan claim’s administrator. You
pay 40% of the allowed amount (after a separate deductible) for services received
Out-of-Network.
Out-of-Network providers can also balance bill you for any difference between their
billed charge and the allowed amount.
Emergency Services – Emergency services are covered everywhere. However, Out-of-Network providers may balance bill the difference between the allowed amount and the billed charge.
Deductible – The amount you pay each benefit plan year before the Plan begins to pay.
Copayment - A fixed dollar amount you pay for a covered service that a member is responsible for paying. The Medical Plan pays the remaining allowed amount.
Coinsurance – A percentage of the allowed amount for covered charges you pay, after paying any applicable deductible.
Out-of-Pocket Maximum - The maximum amount of money you pay toward the cost of covered health care services. Out-of-Pocket expenses include deductibles, copayments, and coinsurance.
Important: Verify the network status of your providers. This is an integral cost savings component of each of your plan choices.
 Medical Plan (optional)
Medical Plan (optional)
Administered by BlueCross BlueShield of Montana
1-800-820-1674 or 406-447-8747
Choices offers a Medical Plan for Retirees and their eligible dependents.
Continuation of enrollment in the Medical Plan is a one-time opportunity for Retirees (and their eligible dependents) at retirement. Coverage is permanently forfeited if the Retiree fails to continue enrollment, cancels Medical coverage, or fails to pay premiums. Note: A legal spouse reaching age 65 is not a qualifying event for re-enrolling in Medical coverage.
| Monthly Medical Plan Rates | |
|---|---|
| Retiree/Survivor Only | $368 |
| Retiree + One | $1,354 |
| Retiree + Two or More | $1,845 |
| Retiree + Spouse (Medicare primary) | $736 |
| Retiree + Spouse (Medicare primary) + Child(ren) | $1,219 |
| Survivor + Child(ren) |
$851 |
Medical Plan Costs- FY2022
| Medical Plan In-Network |
Medical Plan |
|
|---|---|---|
| Annual Deductible Applies to all covered services, unless otherwise noted or copayment is indicated. |
$1,250/Individual $2,500/Family |
Separate $2,500/Individual Separate $5,000/Family |
| Copayment (outpatient office visits) Primary Care Physician Visit (PCP) Specialty Provider Visit |
$30 copay $50 copay |
N/A N/A |
| Coinsurance Percentages (% of allowed charges member pays) |
30% | 40% |
|
Annual Out-of-Pocket Maximum (Maximum amount paid by member in a benefit plan year for covered services; includes deductibles, copays, and coinsurance) |
$4,350/Individual $8,700/Family |
Separate $6,000/Individual Separate $12,000/Family |
*Services from an Out-of-Network provider have separate deductibles, % coinsurance,
and Out-of-Pocket maximums.
An Out-of-Network provider can balance bill the difference between the allowed amount
and the billed charge.
Examples of Medical costs to Plan and Member - Primary Care Physician Visit
Benefit Plan Year July 1 – June 30
(In-Network) Jack’s Plan deductible is $1,250, his coinsurance is 30%, and his Out-of-Pocket max is $4,350.
Jack has not reached his deductible yet and he visits the doctor and has lab work. He pays $30 for the office visit and 100% of the allowed amount for covered lab charges. For example, Jack’s doctor visit totals $1,000. The office visit is $150 and lab work is $850. The Plan allows $100 for the office visit and $400 for the lab work. Jack pays $30 for the office visit and $400 for the lab work. The Plan pays $70 for the office visit and $0 for the lab work. The In-Network provider writes off $500.
Jack has seen the doctor several times and reaches his $1,250 In-Network deductible. His plan pays some of the costs of his next visit. He pays $30 for the office visit and 30% of the allowed amount for lab work and the Plan pays the remainder of the office visit + 70% of the allowed amount. For example, Jack’s doctor visit totals $1,000. The office visit is $150 and lab work is $850. The Plan allows $100 for the office visit and $400 for the lab work. Jack pays $30 for the office visit and $120 for the lab work. The Plan pays $70 for the office visit and $280 for the lab work. The In-Network provider writes off $500.
Jack reaches his $4,350 Out-of-Pocket maximum. Jack has seen his doctor often and paid $4,350 total (deductible + coinsurance + copays). The Plan pays 100% of the allowed amount for covered charges for the remainder of the benefit plan year. For example, Jack’s doctor visit totals $1,000. The office visit is $150 and lab work is $850. The Plan allows $100 for the office visit and $400 for the lab work. Jack pays $0 and the Plan pays $500. The In-Network provider writes off $500.
(Out-of-Network) Jack’s Plan deductible is $2,500, his coinsurance is 40%, and his Out-of-Pocket max is $6,000.
Jack has not reached his deductible yet and he visits the doctor. He pays 100% of the provider charge. Only allowed amounts apply to his deductible. For example, the provider charges $1,000. The Plan allowed amount is $500. $500 applies to Jack’s Out-of-Network deductible. Jack must pay the provider the full $1,000.
Jack has seen the doctor several times and reaches his $2,500 Out-of-Network deductible. His plan pays some of the costs of his next visit. He pays 40% of the allowed amount and any difference between the provider charge and the Plan allowed amount. The Plan pays 60% of the allowed amount. For example, the provider charges $1,000. The Plan allowed amount is $500. Jack pays 40% of the allowed amount ($200) + the difference between the provider charge and the Plan allowed amount ($500). Jack’s total responsibility is $700. The Plan pays 60% of the allowed amount ($300).
Jack reaches his $6,000 Out-of-Pocket maximum. Jack has seen his doctor often and paid $6,000 total (deductible + coinsurance). The Plan pays 100% of the allowed amount for covered charges for the remainder of the benefit plan year. Jack pays the difference between the provider charge and the allowed amount. For example, the provider charges $1,000. The Plan allowed amount is $500. Jack pays $500 and the Plan pays $500.
| Services | In-Network Copay/Coinsurance | Out-of-Network Coinsurance |
|---|---|---|
| Hospital Inpatient Services Pre-Certification of non-emergency inpatient hospitalization is strongly recommended | ||
| Room & Board Charges | 30% | 40% |
| Ancillary Services | 30% | 40% |
|
Surgical Services (See Summary Plan Description for surgeries requiring prior authorization) |
30% | 40% |
| Hospital Outpatient Services | ||
| Outpatient Services | 30% | 40% |
| Outpatient Surgi-Center Services | 30% | 40% |
| Physician/Professional Provider Services (not listed elsewhere) | ||
|
Primary Care Physician (PCP) Office Visit - Includes Telemedicine and Naturopathic visits |
$30 copay/visit for office visit only - lab, x-ray & other procedures are subject to deductible/coinsurance |
40% Note: There is no network for Naturopaths, |
|
Specialty Provider Office Visit - Includes Telemedicine visits |
$50 copay/visit for office visit only - lab, x-ray & other procedures are subject to deductible/coinsurance |
40% |
| Inpatient/Outpatient Physician Services | 30% | 40% |
| Lab/Ancillary/Misc. Services | 30% | 40% |
| Eye Exam (preventive or medical) |
0% one/yr |
40% one/yr |
| Second Surgical Opinion |
0%/visit for office visit only - lab, x-ray & other procedures are subject to deductible/coinsurance |
40% |
| Emergency Services | ||
| Ambulance Services for Medical Emergency | $200 copay/transport | $200 copay/transport |
| Emergency Room Charges |
$250 copay/visit for room charges only - lab, x-ray |
$250 copay/visit for room charges only - lab, x-ray |
| Professional Provider Services | 30% | 30% |
| Urgent Care Services | ||
| Facility/Professional Services |
$75 copay/visit for room charges only - lab, x-ray |
$75 copay/visit for room charges only - lab, x-ray |
| Lab & Diagnostic Services | 30% | 30% |
| Maternity Services | ||
| Hospital Services | 30% | 40% |
| Physician Services (delivery & inpatient) | 30% (waived if enrolled in WellBaby Program within first trimester) |
40% |
| Prenatal Office Visit | 30% copay/visit (waived if enrolled in WellBaby Program within first trimester) |
40% |
| Preventive Services | ||
|
Preventive screenings/immunizations |
0% (limited to Preventive Services Other preventive services subject to deductible and coinsurance) |
40% |
| Mental Health/Chemical Dependency Services | ||
| Inpatient Services (Pre-Certification is recommended) |
30% | 40% |
| Outpatient Visit (this is a combined max of 4 visits at $0 copay for mental health and chemical dependency services) - Includes Telemedicine visits |
First 4 visits $0 copay, then $30 copay/visit |
40% |
|
Psychiatrist Visit - Includes Telemedicine visits |
$50 copay/visit | 40% |
| Rehabilitative Services Physical, Occupational, Speech, Cardiac, Respiratory, Pulmonary, and Massage Therapy; Acupuncture; and Chiropractic | ||
|
Inpatient Services (Pre-Certification is recommended) |
30% Max: 30 days/yr |
40% Max: 30 days/yr |
| Outpatient Visit (this is a combined max of 60 visits for all outpatient rehabilitative services) - Includes Telemedicine visits |
$30 copay/visit |
40% Note: There is no network for |
| Extended Care Services | ||
| Home Health Care Visit (Prior Authorization is recommended) |
$30 copay/visit Max: 30 visits/yr |
40% Max: 30 visits/yr |
| Hospice Services | 30% Max: 6 months |
40% Max: 6 months |
|
Skilled Nursing Facility Services (Prior Authorization is recommended) |
30% Max: 30 days/yr |
40% Max: 30 days/yr |
| Miscellaneous Services | ||
| Allergy Shots |
$50 copay/visit deductible & coinsurance waived |
40% |
| Durable Medical Equipment, Prosthetic Appliances & Orthotics (Prior Authorization is required for amounts greater than $2,500) |
30% Max: $200 for foot orthotics |
40% Max: $200 for foot orthotics |
| PKU Supplies (Includes treatment & medical foods) |
0% (no deductible) | 40% |
| Dietary/Nutritional Counseling Visit - Includes Telemedicine visits |
First 8 visits $0 copay, |
40% |
| Obesity Management (Prior Authorization required) |
30% Must be enrolled in Take Control for non-surgical treatment |
40% |
|
TMJ Services (Prior Authorization required) |
30% Surgical treatment only |
40% |
| Organ Transplants | ||
| Transplant Services (Prior Authorization required) |
30% | 40% |
| Travel Reimbursement | ||
| Travel reimbursement for patient only - If services are not available in local area (Prior Authorization required) |
0% up to $1,500/yr. |
0% up to $1,500/yr. |
| Wellness Program | ||
| Preventive Health Screenings Healthy Lifestyle Education & Support |
See Wellness Program information | |
| WellBaby Program | ||
|
Take Control Lifestyle Mgmt. Program Diabetes, Weight Loss, High Cholesterol, Tobacco Use, High Blood Pressure |
||
Reminder:
Deductible applies to all covered services unless otherwise indicated or a copay applies.
Out-of-Network providers can balance bill the difference between their billed charge
and the allowed amount.
Preventive Services
1. What Services are Preventive?
The MUS Medical Plan provides preventive care coverage that complies with the federal health care reform law, the Patient Protection and Affordable Care Act (PPACA). Services designated as preventive care include:
- periodic wellness visits
- certain designated screenings for symptom- free or disease-free individuals and
- designated routine immunizations.
When preventive care is provided by In-Network providers, services are reimbursed at 100% of the allowed amount, without application of deductible, coinsurance, or copay. Services from an Out-of-Network provider have a 40% coinsurance and a separate deductible and Out-of-Pocket maximum. An Out-of-Network provider can balance bill the difference between the allowed amount and the billed charge.
The PPACA has used specific resources to identify the preventive services that require coverage: U.S. Preventive Services Task Force (USPSTF) A and B recommendations and the Advisory Committee on Immunization Practices (ACIP) recommendations adopted by the Center for Disease Control (CDC). Guidelines for preventive care for infants, children, and adolescents, supported by the Health Resources and Services Administration (HRSA), come from two sources: Bright FuturesRecommendations for Pediatric Health Care and the Uniform Panel of the Secretary’s Advisory Committee on Heritable Disorders in Newborns and Children.
2. Important Tips
- Accurate coding for preventive services by your health care provider is the key to accurate reimbursement by your health care plan. All standard correct medical coding practices should be observed.
- Also of importance is the difference between a “screening” test and a diagnostic, monitoring, or surveillance test. A “screening” test done on an asymptomatic person is a preventive service and is considered preventive even if the test results are positive for disease, but future tests would be considered diagnostic, for monitoring the disease or the risk factors for the disease. A test done because symptoms of disease are present is not a preventive screening and is considered diagnostic.
- Ancillary services directly associated with a “screening” colonoscopy are also considered preventive services. Therefore, the evaluation office visit with the doctor performing the colonoscopy, the colonoscopy procedure, the ambulatory facility fee, anesthesiology (if necessary), and pathology will be reimbursed as preventive, provided they are submitted with accurate preventive coding.
Covered Preventive Services
Note: When preventive care is provided by In-Network providers, services are reimbursed at 100% of the allowed amount, without application of deductible, coinsurance, or copay. Services from an Out-of-Network provider have a 40% coinsurance and a separate deductible and Out-of-Pocket maximum. An Out-of-Network provider can balance bill the difference between the allowed amount and the billed charge.
|
Periodic Exams Appropriate screening tests per Bright Futures and other sources |
|
|
Well-Child Care |
Age 0 months through 4 yrs (up to 14 visits) Age 5 yrs through 17 yrs (1 visit per benefit plan year) |
|
Adult Routine Exam Exams may include screening/counseling and/or risk factor reduction interventions for depression, obesity, tobacco use/abuse, drug and/or alcohol use/abuse |
Age 18 yrs through 65+ (1 visit per benefit plan year)
|
|
Preventive Screenings |
|
|
Anemia Screening |
Pregnant Women |
|
Bacteriuria Screening |
Pregnant Women |
|
Breast Cancer Screening (mammography) |
Women age 40+ (1 per benefit plan year) |
|
Cervical Cancer Screening (PAP) |
Women age 21 - 65 (1 per benefit plan year) |
|
Cholesterol Screening |
Men age 35+ (age 20 - 35 if risk factors for coronary heart disease are present) Women age 45+ (age 20 - 45 if risk factors for coronary heart disease are present) |
|
Colorectal Cancer Screening |
Fecal occult blood testing; 1 per benefit plan year OR Sigmoidoscopy; every 5 yrs OR Colonoscopy; every 10 yrs |
|
Prostate Cancer Screening (PSA) age 50+ |
1 per benefit plan year (age 40+ with risk factors) |
|
Osteoporosis Screening |
Post-menopausal women age 65+, or age 60+ with risk factors (1 bone density x-ray (DXA)) |
|
Abdominal Aneurysm Screening |
Men age 65 - 75 who have ever smoked (1 screening by ultrasound per benefit plan year) |
|
Diabetes Screening |
Adults with high blood pressure |
|
HIV Screening |
Pregnant women and others at risk |
|
RH Incompatibility Screening |
Pregnant women |
|
Routine Immunizations |
|
|
Diphtheria, tetanus, pertussis (DTaP) (Tdap)(TD), Haemophilus influenza (HIB), Hepatitis A & B, Human Papillomavirus (HPV), Influenza, Measles, Mumps, Rubella (MMR), Meningococcal, Pneumococcal (pneumonia), Poliovirus, Rotavirus, Varicella (smallpox), Zoster (shingles). Influenza and Zoster (Shingles) vaccinations are reimbursed at 100% via the Navitus Pharmacy benefit. For recommended immunization schedules for all ages, visit the CDC website at www.cdc.gov/vaccines/index.html |
|
Prescription Drug Plan
(included in Medical Plan)
Your prescription drug coverage is managed by Navitus Health Solutions.
Who is eligible?
The Prescription Drug Plan (PDP) is a benefit for all benefits eligible Montana University System Benefit Plan enrollees and their eligible dependents. Any member enrolled in the Medical Plan will automatically receive Navitus Health Solutions prescription drug coverage. There is no separate premium and no deductible for prescription drugs.
To determine your drug tier level and copay amount before going to the pharmacy, consult the Drug Schedule of Benefits, log into the Navitus Member Portal at www.navitus.com, or call Navitus Customer Care.
The Navitus Drug Formulary List and Pharmacy Directory can be found online at www.navitus.com. You will need to register on the Navitus Navi-Gate for Members web portal to access the MUS-specific drug formulary (preferred drug list), drug tier level, and pharmacy directory. If you have questions regarding the drug formulary list or pharmacy directory, please contact Navitus Customer Care.
How do I fill my prescriptions?
Prescription drugs may be obtained through the Plan at either a local retail pharmacy (up to a 34 or 90-day supply) or through a mail order pharmacy (90-day supply). Members who use maintenance medications can experience a significant cost-savings when filling their prescriptions for a 90-day supply.
Retail Pharmacy Network
NOTE: CVS/Target pharmacies are not part of the Montana University System Pharmacy Plan network. If you choose to use these pharmacies, you will be responsible for all charges. This is not applicable to Navitus MedicareRx enrollees.
Mail Order Pharmacies
Ridgeway, Costco, and miRx Pharmacies administer the mail order pharmacy program. If you are new to the mail order program, you can register online.
 Specialty Pharmacy
Specialty Pharmacy
The preferred Specialty Pharmacy is Lumicera Health Services. Lumicera helps members who are taking prescription drugs that require special handling and/or administration to treat certain chronic illnesses or complex conditions by providing services that offer convenience and support. Ordering new prescriptions with this specialty pharmacy is simple, just call a Patient Care Specialist to get started at 1-855-847-3553.
You can also find a list of Lumicera specialty pharmacy Frequently Asked Questions (FAQs).
Medicare Part D Plan
The Medicare Retiree Prescription Drug Plan, Navitus MedicareRx, is a Medicare Part D prescription drug plan (PDP). Like all Medicare Part D plans, this Medicare prescription drug plan is approved by Medicare and run by a private company.
- Enrollment in another Medicare Part D drug plan is not permitted.
- MUS Medicare primary Retiree Plan members cannot be covered on another MUS Medicare primary Retiree Plan as a legal spouse (dual enrollment).
- Medicare eligible retiree members must be enrolled in BOTH Medicare Part A and B to be eligible for this drug plan and to remain on the Montana University System Medical benefit plan.
|
Drug Schedule of Benefits |
Retail (up to 34-day supply) |
Retail/Mail Order (90-day supply) |
|
Tier $0 (certain preventive medications (ACA, certain statins, metformin, and omeprazole) |
$0 Copay |
$0 Copay |
|
Tier 1 (low cost, high-value generics and select brands that provide high clinical value) |
$15 Copay |
$30 Copay |
|
Tier 2 (preferred brands and select generics that are less cost effective) |
$50 Copay |
$100 Copay |
|
Tier 3 (non-preferred brands and generics that provide the least value because of high cost or low clinical value, or both) |
50% Coinsurance (Does not apply to the |
50% Coinsurance |
|
|
||
|
Tier 4 (Specialty) (specialty medications for certain chronic illnesses or complex diseases) $200 copay if filled at a preferred Specialty pharmacy 50% coinsurance, if filled at a non-preferred Specialty pharmacy (Does not apply to the Out-of-Pocket maximum) |
N/A |
N/A |
|
Out-of-Pocket Maximum |
Individual: $2,150 per benefit plan year Family: $4,300 per benefit plan year |
|
Questions:
Navitus Customer Care
call 24 Hours a Day | 7 Days a wk
Commercial (Non-Medicare Retirees)
Customer Care: 866-333-2757
Member Portal
MedicareRx (Medicare Retirees)
Customer Care: 866-270-3877
Member Portal
Lumicera Health Services
Customer Care: 1-855-847-3553
Monday - Friday 8 a.m. to 6 p.m.
miRx
1-866-894-1496
Monday - Friday 8 a.m. to 6 p.m. MST
 Dental Plan (optional)
Dental Plan (optional)
Administered by Delta Dental: 1-866-579-5717
Choices offers one Dental Plan option for Retirees and their eligible dependents: Select Plan.
Continuation of enrollment in the Dental Plan is a one-time opportunity for Retirees (and their eligible dependents) at retirement. Coverage is permanently forfeited if the Retiree fails to continue enrollment, cancels Dental coverage, or fails to pay premiums. Note: A legal spouse reaching age 65 is not a qualifying event for re-enrolling in Dental coverage.
| Select Plan – Enhanced Coverage | |
|---|---|
| Monthly Dental Plan Rates |
Retiree/Survivor Only $52 |
| Annual Benefit Maximum | $2,000 per covered individual |
|
Diagnostic & Preventive Services |
Twice per benefit plan year: Initial and periodic oral exam |
|
Basic Restorative Services
|
Amalgam filling |
|
Major Dental Services
|
Crown |
|
Orthodontia Services |
Available to all Select Plan covered members. |
Select Plan Benefit Highlights:
Diagnostic & Preventive Services
The Choices Select Plan allows MUS Dental Plan members to obtain diagnostic & preventive services without those costs applying to the annual $2,000 maximum.
Orthodontic Benefits
The Choices Select Plan allows a $1,500 lifetime orthodontic benefit per covered individual. Benefits are paid at 50% of the allowed amount for authorized services. Treatment plans usually include an initial down payment and ongoing monthly fees. If an initial down payment is required, Choices will pay up to 50% of the initial payment, up to 1/3 of the total treatment charge. In addition, Delta Dental (the Dental Plan claims administrator) will establish a monthly reimbursement based on your provider’s monthly fee and your prescribed treatment plan.
Dental Fee Schedule
Dental claims are reimbursed based on a dental fee schedule. The following subsets of the Choices Select Plan fee schedule includes the most common used procedure codes. The fee schedule’s dollar amount is the maximum reimbursement paid by the Plan for the specified procedure code. Covered members are responsible for the difference (if any) between the provider’s billed charge and the fee schedule’s maximum reimbursement amount.
The CDT codes and nomenclature are copyright of the American Dental Association. The
procedures described and maximum allowances indicated on this table are subject to
the terms of the MUS-Delta Dental contract and Delta Dental processing policies. These
allowances may be further reduced due to maximums, limitations, and exclusions.
Please refer to the SPD for complete benefit and fee schedule information (see pg.
35 for availability).
Delta Dental Fee examples
How to select a Delta Dental network dentist that will best suit your needs and your pocketbook! Understand the difference between a PPO and Premier network dentist.
Finding a Delta Dental Network Dentist:
The MUS Dental Plan utilizes a fee schedule so you know in advance exactly how much the Plan will pay for each covered service. It is important to understand that a dentist’s billed charges may be greater than the MUS Plan benefit fee schedule amount, resulting in balance billing. When a dentist contracts with Delta Dental, they agree to accept Delta Dental’s allowed fee as full payment. This allowed fee may be greater than the MUS Plan benefit fee schedule amount in which case, the dentist may balance bill you up to the difference between the allowed fee and the MUS Plan benefit fee schedule amount.
While you have the freedom of choice to visit any licensed dentist under the Plan, you may want to consider visiting a Delta Dental network dentist to reduce your Out-of-Pocket costs.
Montana University System plan members will usually save when they visit a Delta Dental network dentist. Delta Dental Preferred Provider Organization (PPO) network dentists agree to lower levels of allowed fees and therefore offer the most savings. Delta Dental Premier network dentists also agree to a set level of allowed fees, but not as low as with a PPO network dentist. Therefore, when visiting a Premier network dentist, MUS members usually see some savings, just not as much as with a PPO network dentist. The best way to understand the difference in fees is to view the examples below.
Use the Find a Dentist search to help you select a network dentist that is best for you!
The following claim example for an adult cleaning demonstrates how lower Out-of-Pocket patient costs can be achieved when you visit a Delta Dental network dentist. The example compares the patient’s share of costs at each network level below:
|
|
PPO Network |
Premier Network |
Out-of-Network Dentist |
|
What the dentist bills |
$87 |
$87 |
$87 |
|
Dentists allowed fee with Delta Dental |
$57 |
$71 |
No fee agreement with Delta Dental |
|
MUS Plan fee schedule amount |
$83 |
$83 |
$83 |
|
What you pay |
$0 |
$0 |
$4 |
The following claim example for a crown demonstrates how lower Out-of-Pocket patient costs can be achieved when you visit a Delta Dental network dentist. The example compares the patient’s share of costs at each network level below:
|
|
PPO Network |
Premier Network |
Out-of-Network Dentist |
|
What the dentist bills |
$1,000 |
$1,000 |
$1,000 |
|
Dentists allowed fee with Delta Dental |
$694 |
$822 |
No fee agreement with Delta Dental |
|
MUS Plan fee schedule amount |
$423 |
$423 |
$423 |
|
What you pay |
$271 |
$399 |
$577 |
| Procedure Code | Description | Fee Schedule |
|---|---|---|
| D0120 | Periodic oral evaluation – established patient | $44.00 |
| D0140 | Limited oral evaluation – problem focused | $59.00 |
| D0145 | Oral evaluation for a patient under three years of age and counseling with primary caregiver | $47.00 |
| D0150 | Comprehensive oral evaluation – new or established patient | $65.00 |
| D0160 | Detailed and extensive oral evaluation – problem focused, by report | $139.00 |
| D0170 | Re-evaluation – limited, problem focused (established patient; not post-operative visit) | $52.00 |
| D0180 | Comprehensive periodontal evaluation – new or established patient | $72.00 |
| D0190 | Screening of a patient | $28.00 |
| D0191 | Assessment of a patient | $28.00 |
| D0210 | Intraoral – complete series of radiographic images | $122.00 |
| D0220 | Intraoral – periapical first radiographic image | $26.00 |
| D0230 | Intraoral – periapical each additional radiographic image | $20.00 |
| D0240 | Intraoral – occlusal radiographic image | $25.00 |
| D0250 | Extra-oral – 2D projection radiographic image created using a stationary radiation source, and detector | $58.00 |
| D0270 | Bitewing – single radiographic image | $23.00 |
| D0272 | Bitewings – two radiographic images | $41.00 |
| D0273 | Bitewings – three radiographic images | $49.00 |
| D0274 | Bitewings – four radiographic images | $54.00 |
| D0277 | Vertical bitewings – 7 to 8 radiographic images | $75.00 |
| D0310 | Sialography | $411.00 |
| D0320 | Temporomandibular joint arthrogram, including injection | $622.00 |
| D0321 | Other temporomandibular joint radiographic images, by report | $224.00 |
| D0322 | Tomographic survey | $355.00 |
| D0330 | Panoramic radiographic image | $97.00 |
| D1110 | Prophylaxis – adult | $87.00 |
| D1120 | Prophylaxis – child (through age 13) | $58.00 |
| D1206 | Topical application of fluoride varnish (Child through age 18) | $31.00 |
| D1208 | Topical application of fluoride – excluding varnish (Child through age 18) | $28.00 |
| D1351 | Sealant – per tooth (Child through age 15) | $45.00 |
| D1352 | Preventive resin restoration in a moderate to high caries risk patient – permanent tooth (Child through age 15) | $54.00 |
| D1510 | Space maintainer – fixed, unilateral – per quadrant (Child through age 13) | $280.00 |
| D1516 | Space maintainer – fixed – bilateral, maxillary (Child through age 13) | $388.00 |
| D1517 | Space maintainer – fixed – bilateral, mandibular (Child through age 13) | $388.00 |
| D1520 | Space maintainer – removable, unilateral – per quadrant (Child through age 13) | $393.00 |
| D1526 | Space maintainer – removable – bilateral, maxillary (Child through age 13) | $538.00 |
| D1527 | Space maintainer – removable – bilateral, mandibular (Child through age 13) | $538.00 |
| D1551 | Re-cement or re-bond bilateral space maintainer – maxillary | $63.00 |
| D1552 | Re-cement or re-bond bilateral space maintainer – mandibular | $63.00 |
| D1553 | Re-cement or re-bond unilateral space maintainer – per quadrant | $63.00 |
| D1556 | Removal of fixed unilateral space maintainer – per quadrant | $63.00 |
| D1557 | Removal of fixed bilateral space maintainer – maxillary | $63.00 |
| D1558 | Removal of fixed bilateral space maintainer – mandibular | $63.00 |
| D1575 | Distal shoe space maintainer - fixed, unilateral – per quadrant | $239.00 |
| D2140 | Amalgam – one surface, primary or permanent | $93.00 |
| D2150 | Amalgam – two surfaces, primary or permanent | $118.00 |
| D2160 | Amalgam – three surfaces, primary or permanent | $147.00 |
| D2161 | Amalgam – four or more surfaces, primary or permanent | $176.00 |
| D2330 | Resin-based composite – one surface, anterior | $109.00 |
| D2331 | Resin-based composite – two surfaces, anterior | $141.00 |
| D2332 | Resin-based composite – three surfaces, anterior | $170.00 |
| D2335 | Resin-based composite – four or more surfaces or involving incisal angle (anterior) | $209.00 |
| D2391 | Resin-based composite – one surface, posterior | $124.00 |
| D2392 | Resin-based composite – two surfaces, posterior | $159.00 |
| D2393 | Resin-based composite – three surfaces, posterior | $203.00 |
| D2394 | Resin-based composite – four or more surfaces, posterior | $238.00 |
| D2510 | Inlay – metallic – one surface | $292.00 |
| D2520 | Inlay – metallic – two surfaces | $344.00 |
| D2542 | Onlay – metallic – two surfaces (12 years and older) | $419.00 |
| D2610 | Inlay – porcelain/ceramic – one surface | $292.00 |
| D2620 | Inlay – porcelain/ceramic – two surfaces | $335.00 |
| D2642 | Onlay – porcelain/ceramic – two surfaces (12 years and older) | $453.00 |
| D2650 | Inlay – resin-based composite – one surface | $292.00 |
| D2651 | Inlay – resin-based composite – two surfaces | $335.00 |
| D2662 | Onlay – resin-based composite – two surfaces (12 years and older) | $371.00 |
| D2740 | Crown – porcelain/ceramic substrate | $492.00 |
| D2750 | Crown – porcelain fused to high noble metal | $463.00 |
| D2751 | Crown – porcelain fused to predominantly base metal | $410.00 |
| D2780 | Crown – ¾ cast high noble metal | $516.00 |
| D2783 | Crown – ¾ porcelain/ceramic | $488.00 |
| D2790 | Crown – full cast high noble metal | $515.00 |
| D2930 | Prefabricated stainless steel crown – primary tooth | $186.00 |
| D2931 | Prefabricated stainless steel crown – permanent tooth | $222.00 |
| D2932 | Prefabricated resin crown | $221.00 |
| D2933 | Prefabricated stainless steel crown with resin window | $222.00 |
| D2940 | Protective restoration | $70.00 |
| D2950 | Core buildup, including any pins when required | $151.00 |
| D3110 | Pulp cap – direct (excluding final restoration) | $49.00 |
| D3220 | Therapeutic pulpotomy (excluding final restoration) – removal of pulp coronal to the dentinocemental junction and application of medicament | $121.00 |
| D3330 | Endodontic therapy, molar tooth (excluding final restoration) | $858.00 |
| D3346 | Retreatment of previous root canal therapy – anterior | $759.00 |
| D3347 | Retreatment of previous root canal therapy – premolar | $828.00 |
| D3410 | Apicoectomy – anterior | $762.00 |
| D3425 | Apicoectomy – molar (first root) | $765.00 |
| D3430 | Retrograde filling – per root | $153.00 |
| D4210 | Gingivectomy or gingivoplasty – four or more contiguous teeth or tooth bounded spaces per quadrant | $364.00 |
| D4249 | Clinical crown lengthening – hard tissue | $455.00 |
| D4260 | Osseous surgery (including elevation of a full thickness flap and closure) – four or more contiguous teeth or tooth bounded spaces per quadrant | $1,000.00 |
| D4270 | Pedicle soft tissue graft procedure | $620.00 |
| D4341 | Periodontal scaling and root planing – four or more teeth per quadrant | $170.00 |
| D4342 | Periodontal scaling and root planing – one to three teeth per quadrant | $112.00 |
| D4346 | Scaling in presence of generalized moderate or severe gingival inflammation – full mouth, after oral evaluation | $95.00 |
| D4355 | Full mouth debridement to enable a comprehensive oral evaluation and diagnosis on a subsequent visit | $104.00 |
| D4910 | Periodontal maintenance | $96.00 |
| D5110 | Complete denture – maxillary | $658.00 |
| D5120 | Complete denture – mandibular | $662.00 |
| D5130 | Immediate denture – maxillary | $764.00 |
| D5140 | Immediate denture – mandibular | $777.00 |
| D5211 | Maxillary partial denture – resin base (including retentive/clasping materials, rests, and teeth) | $442.00 |
| D5212 | Mandibular partial denture – resin base (including retentive/clasping materials, rests, and teeth) | $535.00 |
| D5213 | Maxillary partial denture – cast metal framework with resin denture bases (including retentive/clasping materials, rests and teeth) | $703.00 |
| D5214 | Mandibular partial denture – cast metal framework with resin denture bases (including retentive/clasping materials, rests and teeth) | $695.00 |
| D5225 | Maxillary partial denture – flexible base (including any clasps, rests and teeth) | $488.00 |
| D5226 | Mandibular partial denture – flexible base (including any clasps, rests and teeth) | $617.00 |
| D5411 | Adjust complete denture – mandibular | $32.00 |
| D5611 | Repair resin partial denture base, mandibular | $89.00 |
| D5612 | Repair resin partial denture base, maxillary | $89.00 |
| D5640 | Replace broken teeth – per tooth | $99.00 |
| D5650 | Add tooth to existing partial denture | $114.00 |
| D5660 | Add clasp to existing partial denture – per tooth | $160.00 |
| D5710 | Rebase complete maxillary denture | $320.00 |
| D5711 | Rebase complete mandibular denture | $320.00 |
| D5720 | Rebase maxillary partial denture | $314.00 |
| D5721 |
Rebase mandibular partial denture |
$360.00 |
| D5820 | Interim partial denture (maxillary) | $216.00 |
| D5821 | Interim partial denture (mandibular) | $233.00 |
| D5850 | Tissue conditioning, maxillary | $51.00 |
| D5851 | Tissue conditioning, mandibular | $51.00 |
| D5863 | Overdenture – complete maxillary | $930.00 |
| D6010 | Surgical placement of implant body: endosteal implant | $855.00 |
| D6210 | Pontic – cast high noble metal | $622.00 |
| D6212 | Pontic – cast noble metal | $365.00 |
| D6214 | Pontic – titanium and titanium alloys | $528.00 |
| D6240 | Pontic – porcelain fused to high noble metal | $491.00 |
| D6241 | Pontic – porcelain fused to predominantly base metal | $425.00 |
| D6242 | Pontic – porcelain fused to noble metal | $463.00 |
| D6740 | Retainer crown – porcelain/ceramic | $492.00 |
| D6750 | Retainer crown – porcelain fused to high noble metal | $499.00 |
| D6752 | Retainer crown – porcelain fused to noble metal | $490.00 |
| D6790 | Retainer crown – full cast high noble metal | $498.00 |
| D6791 | Retainer crown – full cast predominantly base metal | $402.00 |
| D6794 | Retainer crown – titanium and titanium alloys | $548.00 |
| D7111 | Extraction, coronal remnants – primary tooth | $68.00 |
| D7140 | Extraction, erupted tooth or exposed root (elevation and/or forceps removal) | $115.00 |
| D7210 | Extraction, erupted tooth requiring removal of bone and/or sectioning of tooth, and including elevation of mucoperiosteal flap if indicated | $199.00 |
| D7220 | Removal of impacted tooth – soft tissue | $237.00 |
| D7230 | Removal of impacted tooth – partially bony | $283.00 |
| D7240 | Removal of impacted tooth – completely bony | $326.00 |
| D7850 | Surgical discectomy, with/without implant | $1,500.00 |
| D7860 | Arthrotomy | $1,500.00 |
| D7971 | Excision of pericoronal gingiva | $120.00 |
| D9110 | Palliative (emergency) treatment of dental pain – minor procedure | $70.00 |
| D9120 | Fixed partial denture sectioning | $86.00 |
| D9222 | Deep sedation/general anesthesia – first 15 minutes | $280.00 |
| D9223 | Deep sedation/general anesthesia – each subsequent 15 minute increment | $134.00 |
| D9239 | Intravenous moderate (conscious) sedation/analgesia – first 15 minutes | $252.00 |
| D9243 | Intravenous moderate (conscious) sedation/analgesia – each subsequent 15 minute increment | $111.00 |
| D9310 | Consultation – diagnostic service provided by dentist or physician other than requesting dentist or physician | $67.00 |
| D9942 | Repair and/or reline of occlusal guard | $40.00 |
| D9944 | Occlusal guard – hard appliance, full arch | $273.00 |
| D9945 | Occlusal guard – soft appliance, full arch | $146.00 |
| D9946 | Occlusal guard – hard appliance, partial arch | $320.00 |
| D9950 | Occlusion analysis – mounted case | $187.00 |
| D9951 | Occlusal adjustment – limited | $51.00 |
| D9952 | Occlusal adjustment – complete | $406.00 |
Vision Hardware Plan (optional)
Administered by BlueCross BlueShield of Montana - 1-800-820-1674 or 1-406-447-8747
Choices offers a Vision Hardware Plan for Retirees and their eligible dependents.
Continuation of enrollment in the Vision Hardware Plan is a one-time opportunity for Retirees (and their eligible dependents) at retirement. Coverage is permanently forfeited if the Retiree fails to continue enrollment, cancels Vision Hardware coverage, or fails to pay premiums. Note: A legal spouse reaching age 65 is not a qualifying event for re-enrolling in Vision Hardware coverage.
Using Your Vision Hardware Plan Benefit
Quality vision care is important to your eye wellness and overall health care. Accessing your Vision Hardware Plan benefit is easy. Simply select your provider, purchase your hardware, and submit your claim form to BlueCross BlueShield of Montana for processing. The optional vision hardware coverage is a hardware benefit only. Eye Exams, whether preventive or medical, are covered under the Medical Plan (see Eye Exam (preventive & medical) in the Schedule of Medical Plan Benefits). Please refer to the Summary Plan Description (SPD) for complete Vision Hardware Plan benefits and plan exclusions.
Monthly Vision Hardware Plan Rates
Retiree/Survivor Only $10.70
Retiree & Spouse $20.20
Retiree/Survivor & Child(ren) $21.26
Retiree & Family $31.18
|
Service/Material |
Coverage |
|---|---|
|
Eyeglass Frame and Lenses: Frame: One eyeglass frame per benefit plan year, in lieu of contact lenses Lenses: One pair of prescription lenses per benefit plan year, in lieu of contact lenses |
Up to $300 allowance toward the purchase of one eyeglass frame and one pair of prescription lenses, including single vision, bifocal, trifocal, progressive lenses; ultraviolet treatment; tinting; scratch-resistant coating; polycarbonate; anti-reflective coating. The Plan member may be responsible for charges at the time of purchase. |
|
Contact Lenses: One purchase per benefit plan year, in lieu of eyeglass frame and prescription lenses |
Up to $200 allowance toward contact lens fitting and the purchase of conventional, disposable, or medically necessary* contact lenses. The Plan member may be responsible for charges at the time of purchase. |
*Contact lenses that are required to treat medical or abnormal visual conditions, including but not limited to eye surgery (i.e., cataract removal), visual perception in the better eye that cannot be corrected to 20/70 through the use of eyeglasses, and certain corneal or other eye diseases.
Filing a claim:
When a Plan member purchases vision hardware, a walk-out statement should be provided by the Provider. This walk-out statement should be submitted to BlueCross BlueShield of Montana for reimbursement, along with a Vision Hardware Claim Form.
MUS Wellness Program (optional)
The Montana University System (MUS) Benefit Plan offers Wellness services to covered adult Medical Plan members (employees, retirees, legal spouse, COBRA enrollees, and covered dependent children over the age of 18).
Preventive Health Screenings
WellChecks: Each campus offers preventive health screenings for adult Medical Plan members called WellChecks. A free basic blood panel and biometric screening are provided at WellCheck, with optional additional tests available at discounted prices. Representatives from MUS Wellness are also present at most WellChecks to answer wellness related questions. Adult Medical Plan members over the age of 18 are eligible for two free WellChecks per benefit plan year (July 1 - June 30). More information regarding WellCheck dates and times in your area.
Online Registration: Online registration is required for all participants for WellCheck appointments. To register go to my.itstartswithme.com.
Lab Tests: Log on to your It Starts With Me account for a complete listing of tests available at WellCheck.
Flu Shots: Are offered FREE in the fall, subject to national vaccine availability. For more information, visit WellCheck & Flu Shots on the Wellness website.
Healthy Lifestyle Education & Support
Quick Help Program:
If you have a quick question regarding health, fitness, or nutrition related topics, send us an email at: wellness@montana.edu. We will do our best to provide the information you need or point you in the right direction if we do not have an answer ourselves! The information given through the Quick Help Program does not provide medical advice, is intended for general educational purposes only, and does not always address individual circumstances.
WellBaby Program:
WellBaby is a pregnancy program designed to help you achieve a healthier pregnancy. Enroll during your first trimester to take advantage of all program benefits. For more information call 406-660-0082.
Take Control Lifestyle Management Program:
Take Control is a health coaching program that believes living well is within everyone’s reach. Take Control offers comprehensive and confidential education and support for the following: Diabetes/Pre-Diabetes, Weight Loss, Tobacco Cessation, High Blood Pressure, High Cholesterol, and Maternal Health for WellBaby participants.
Services provided include monthly health coaching, copay waivers for diabetic supplies and many more.
For details, visit Wellness Take Control or contact Take Control at 1-800-746-2970.
Available to Non-Medicare retirees only
Additional Benefits That Can Be Pre-Authorized by your Health Coach:
Visit with your In-Network primary health care provider (with $0 copay), personal
training, sleep study (deductible/coinsurance waived), additional counseling visits
(with $0 copay).
Stay Connected
For education and updates visit our Blog * Like us on Facebook * Visit the MUS Wellness Website
Additional Benefit Plan Information
Self-Audit Award Program
Be sure to check all medical health care provider bills and Explanation of Benefits (EOBs) from the Medical Plan claims administrator to ensure that charges have not been duplicated or you have been billed for services you did not receive. When you detect billing errors that result in a claims adjustment, the MUS Plan will share the savings with you! You may receive an award of 50% of the savings, up to a maximum of $1,000.
The Self-Audit Award Program is available to all MUS Medical Plan members who identify medical billing errors which:
- Have not already been detected by the Medical Plan claims administrator or reported by the health care provider,
- Involve medical services which are allowable and covered by the MUS Medical Plan, and
- Total $50 or more in errant charges.
To receive the Self-Audit Award, the member must:
- Notify the Medical Plan claims administrator of the error before it is detected by the claims administrator or the health care provider,
- Contact the health care provider to verify the error and work out the correct billing, and
- Have copies of the correct billing sent to the Medical Plan claims administrator for verification, claims adjustment and calculation of the Self-Audit Award.
Summary Plan Description (SPD)
All Montana University System (MUS) Plan participants have the right to obtain a current copy of the Summary Plan Description (SPD). Despite the use of “summary” in the title, this document contains the full legal description of the Plan’s medical, dental, vision hardware, and prescription drug benefits and should always be consulted when a specific question arises about the Plan.
Plan participants may request a hard copy of the SPD by contacting their campus Human Resources/Benefits Office or the MUS Benefits Office at 1-877-501-1722. The SPD is also available online on the MUS Choices website.
Summary of Benefits and Coverage (SBC)
The SBC document, which is required by PPACA, will outline what the MUS Medical Plan covers and what the cost share is for the member and the Plan for covered health care services.
Eligibility and enrollment rules for coverage in the Montana University System Group Benefit Plan for
participants and their eligible dependents (who are NOT active employees within MUS), are published in the MUS Summary Plan Description in these sections:
- Eligibility
- Enrollment, Changes in Enrollment, Effective Dates of Coverage
- Leave, Layoff, Coverage Termination, Re-Enrollment, Surviving Dependent, and Retirement Options
- Continuation of Coverage Rights under COBRA
Each employee and former employee are responsible for understanding the rights and
responsibilities for
themselves and their eligible dependents for maintaining enrollment in the Montana
University System
Group Benefit Plan.
Retirees eligible for Medicare and paying Medicare Retiree monthly premium rates, as published in the Choices Retiree Workbook, are required to be continuously enrolled in BOTH Medicare Part A and Medicare Part B.
Coordination of Benefits: Persons covered by a health care plan through the Montana University System AND by another non-liability health care coverage plan, whether private, employer-based, governmental (including Medicare and Medicaid), are subject to coordination of benefits rules as specified in the Summary Plan Description, Coordination of Benefits section. Rules vary from case to case by the circumstances surrounding the claim and by the active or retiree status of the member. In no case will more than 100% of a claim’s allowed amount be paid by the sum of all payments from all applicable coordinated insurance coverages.
Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) Notice
The Montana University System Group Benefit Plan has a duty to safeguard and protect the privacy of all Plan members’ personally identifiable health information that is created, maintained, sent, or received by the Plan.
The HIPAA Notice can be accessed on the MUS Choices website at www.choices.mus.edu/Publication_Notices.html.
The Montana University System Group Benefit Plan contracts with individuals or entities, known as Business Associates, who perform various functions on the Plan’s behalf such as claims processing and other
health-related services associated with the Plan, including claims administration or to provide support services, such as medical review or pharmacy benefit management services, etc.
The Montana University System’s self-insured Group Benefit Plan, in administering Plan benefits, shares and receives personally identifiable medical information concerning Plan members as required by law and for routine transactions concerning eligibility, treatment, payments, wellness programs (including WellChecks), lifestyle management programs (e.g., Take Control), healthcare operations, claims processing (including review of claims payments or denials, appeals, health care fraud and abuse detection, and compliance). Information concerning these categories may be shared, without a Plan participant’s written consent, between authorized MUS Benefits Division employees and MUS Business Associates, the participant’s providers, or legally authorized governmental entities.
Glossary
Allowed Amount
A set dollar allowance for procedures/services that are covered by the Plan.
Balance Billing
This amount is the difference between the provider’s billed charge and the allowed amount for services provided by an Out-of-Network provider or the billed amount for a non-covered service.
Benefit Plan Year
The period starting July 1 and ending June 30.
Certification/Pre-Certification
A determination by the Medical Plan claims administrator that a specific service - such as an inpatient hospital stay - is medically necessary. Pre-Certification is done in advance of a non-emergency admission by contacting the Medical Plan claims administrator.
Coinsurance
A percentage of the allowed amount for covered health care services that a member is responsible for paying, after paying any applicable deductible. For example, if Jack has met his deductible for In-Network medical costs ($1,250), he pays 30% of the allowed amount up to the Out-of-Pocket Maximum and the Plan pays 70%.
Copayment
A fixed dollar amount the member pays for a covered health care service, usually at the time the member receives the service. The Plan pays the remaining allowed amount.
Covered Charges
Charges for health care services that are determined to be medically necessary and are eligible for payment under the Plan.
Deductible
A set dollar amount that a member must pay for covered health care services before the Medical Plan pays. The deductible applies to the benefit plan year (July 1 through June 30). For example, Jack’s deductible is $1,250. Jack pays 100% of the allowed amount until his deductible has been met.
Diagnostic
A type of service that includes tests or exams usually performed for monitoring a disease or condition which you have signs, symptoms, or prevailing medical history for.
Emergency Services
Evaluation and treatment of an emergency medical condition (illness, injury, or serious condition). Emergency Services are covered everywhere; however, Out-of-Network providers may balance bill the difference between the allowed amount and the billed charge.
Fee Schedule
A fee schedule is a complete listing of fees used by the Plan to reimburse providers and suppliers for providing selected health care services. The comprehensive listing of fee maximums is used to reimburse a provider on a fee-for-service or flat-fee basis.
In-Network Provider
A provider who has a participating contract with the Plan claims administrator to provide health care services for Plan members and to accept the allowed amount as payment in full. Also called “preferred provider” or “participating provider”. Members will pay less Out-of-Pocket expenses if they see an In-Network provider.
Out-of-Network Provider
Any provider who provides services to a member but does not have a participating contract with the Plan claims administrator. Also called “non-preferred provider” or non-participating provider”. Members will pay more Out-of-Pocket expenses if they see an Out-of-Network provider.
Out-of-Pocket Maximum
The maximum amount of money a member pays toward the cost of covered health care services.
Out-of-Pocket expenses include deductibles, copayments, and coinsurance. For example, Jack reaches his $4,350 Out-of-Pocket Maximum. Jack has seen his doctor often and paid $4,350 total (deductible + coinsurance + copays). The Plan pays 100% of the allowed amount for covered charges for the remainder of the benefit plan year. Balance billing amounts (the difference between Out-of-Network provider billed charges and the allowed amount) do not apply to the Out-of-Pocket Maximum.
Plan
Healthcare benefits coverage offered to members through the employer to assist with the cost of covered health care services.
Preventive Services
Routine health care, including screenings and exams, to prevent or discover illnesses, disease, or other health problems.
Prior Authorization
Routine health care, including screenings and exams, to prevent or discover illnesses, disease, or other health problems.
PPACA
The Patient Protection and Affordable Care Act (PPACA) – also known as the Affordable Care Act or ACA – is the landmark health reform legislation passed by the 111th Congress and signed into law by President Barack Obama in March 2010. The legislation includes a list of health-related provisions that took effect in 2010.
Primary Care Physician
A physician (M.D. – Medical Doctor or D.O. – Doctor of Osteopathic Medicine, nurse practitioner, clinical nurse specialist or physician assistant) who directly provides or coordinates a range of health care services for or helps access health care services for a patient.
Screening
A type of preventive service that includes tests or exams to detect the presence of something, usually performed when you have no symptoms, signs, or prevailing medical history of a disease or condition.
Specialist
A physician specialist who focuses on a specific area of medicine to diagnose, manage, prevent, or treat certain types of symptoms and conditions.
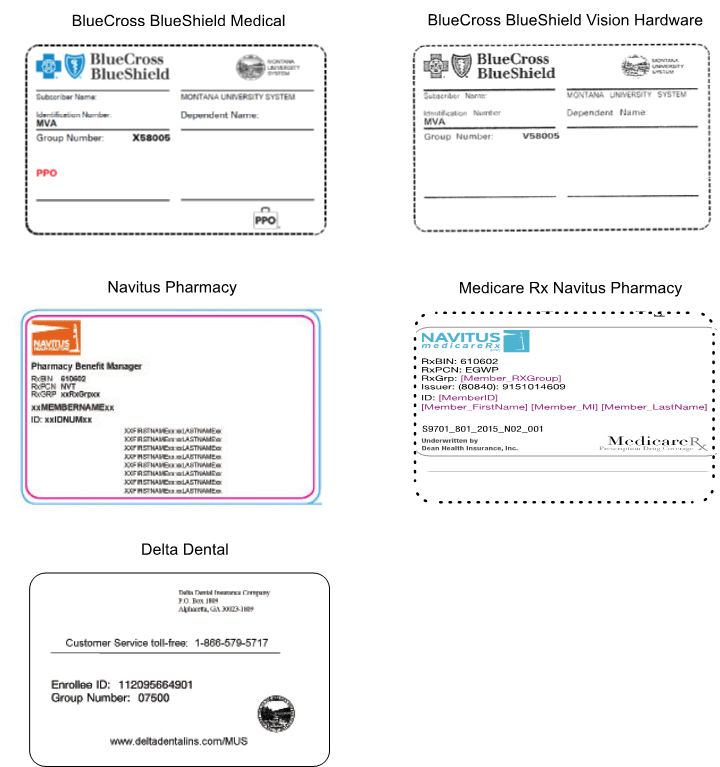
Insurance Card Examples
Resources
Montana University System Benefits Office
Office of the Commissioner of Higher Education
877-501-1722 * Fax (406) 449-9170
MEDICAL PLAN & VISION HARDWARE PLAN
BLUECROSS BLUESHIELD OF MONTANA
800-820-1674 or 406-447-8747
DENTAL PLAN
DELTA DENTAL
866-579-5717
PRESCRIPTION DRUG PLAN
Navitus Commercial Plan (NON-MEDICARE RETIREES)
866-333-2757
Navitus MedicareRx Plan (MEDICARE RETIREES)
866-270-3877
RIDGEWAY MAIL ORDER PHARMACY
800-630-3214
Fax: 406-642-6050
COSTCO MAIL ORDER PHARMACY
800-607-6861
Fax: 888-545-4615
miRx MAIL ORDER PHARMACY
866-894-1496
Fax: (406) 869-6552
LUMICERA HEALTH SERVICES
855-847-3553
